

Approved as a medical device by the Israeli Ministry of Health
Res #3198004ifoi
Sterisent was conceived on our farm in Israel following our belief in a simple close to nature life. After years of development and personal use It was first given out to friends and family . The feedback was so positive we started the marketing campaign in hospitals and among professional caregivers.
live green,
innovate greener
Time and again we hit the brick wall of skepticism, even after presenting the detailed lab reports. The reaction was total disbelief that such a solution produced only from water, pure salt and our state of the art electric reactor could actually eradicate 99.9% of known pathogens including antibiotic resistant super bug
During a social event we ran into a well known epidemiologist who was willing to give it a try. We delivered the goods to his clinic in Israel’s biggest and world known hospital only to receive a message the next day he wouldn't use it and to take it back because he didn't believe it works. There was only one doctor who tried it on his patients suffering from hard to heal wounds and was totally dazzled by the result. His bravery was awarded by a lifetime of free supply
managing infection
Managing infection has always been part of wound care clinical practice guidelines because infection episodes not only halt the wound-healing process, but also can lead to complications, including hospitalization, loss of tissue, amputation of feet or legs and even death.
HOCl was introduced in World War 1 but its use was eclipsed by the widespread introduction of antibiotics
However, in recent years as antibiotic resistance and questions about the cytotoxicity of antiseptics have impacted wound care practice, interest has increased regarding more advanced HOCl solutions introduced into the marketplace.
Stabilized Sterisent has managed to overcome the problem of pure HOCl having a very short half life that in a matter of days and even hours disassociates into water and chlorine. With our propriety state of the art electro chemical reactor we guarantee 1.5 years of safety and efficacy.
means of application
AT HOME: from treating cuts and burns to eliminating acne and sabirua up to baby rush and
tstore it in yor beatch bag to tackle those nasty jellyfifh attacks and subburns
negative pressure wound therapy (NPWT) has emerged as a common treatment for acute and chronic wounds, including diabetic wounds, pressure ulcers, and burns. In simple terms, NPWT refers to any device that tightly seals the wound creating a near airtight environment to which a vacuum can be applied resulting in a series of biological reactions that enhance wound healing. Fluid is instilled into the wound through a port on the connecting tube to enhance wound healing,
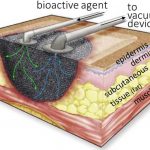
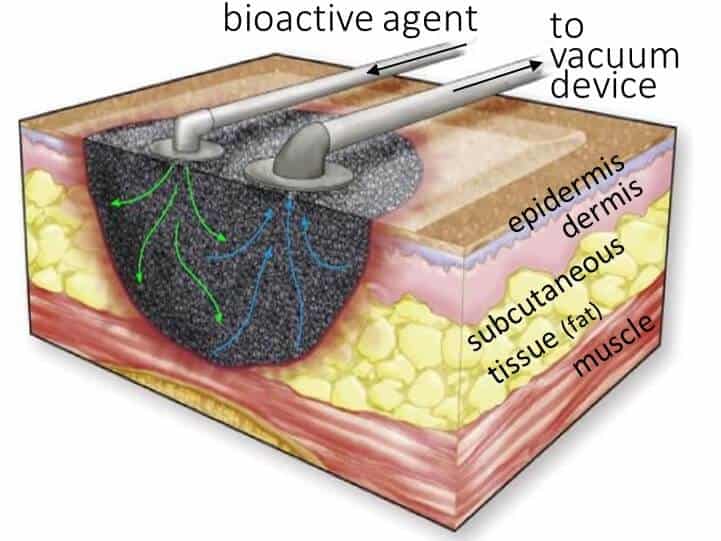
Sterisent is a better solution than saline used today as it was found to decrease bacterial load and induce early initiation of granulation tissue formation. Negative pressure wound therapy (NPWT) is a method of drawing out fluid and infection from a wound to help it heal. Sterisent is a better solution than saline used today as it was found to decrease bacterial load and induce early initiation of granulation tissue formation. Negative pressure wound therapy (NPWT) is a method of drawing out fluid and infection from a wound to help it heal. drawing out fluid and infection from a wound to help it heal. A special dressing (bandage) is sealed over the wound and a gentle vacuum pump is attached. At the wound site, negative pressure wound therapy promotes wound healing and closure by removing excess fluids that can hamper the success of the treatment
Perhaps the most remarkable property of HOCl is its ability to destroy biofilms.Identifying and managing biofilms have become two of the most important aspects of wound care. Biofilms can have a significant impact on wound healing, by contributing to bacterial infection, inflammation, and delayed wound healing.1 These issues make reducing biofilm presence a critical component of effective wound care
Biofilms are microbial communities, generally composed of bacteria, fungi, and other microorganisms. Although the organisms themselves are microscopic, once biofilms mature they often form a visible protective matrix that attaches the community to the surface.
Underdeveloped biofilms may be difficult to identify, but as they grow larger, they are much more easily visible, often taking the appearance of a viscous, shiny film. This film protects the microorganisms living within it and prevents antibodies from reaching them. nearly two thirds of chronic acquire overgrowth characterized differ from planktonic microbial colonies in terms of structure, gene expression ,antibiotic resistance, and host interaction largely because 5% to 30% of the biofilm is composed of extracellular polymeric substances, such as glycoproteins. Moreover, biofilms can contain anaerobes, which often are missed by classical culture techniques and grow by contiguous spreading or shedding of planktonic bacteria, seeding onto surrounding surfaces, and resulting in infection dissemination. Biofilms are also notorious for their persistence, being resistant to the host immune system, systemic antibiotics, and topical antimicrobials. Current biofilm debridement methods rely on time consuming and aggressive surgical procedures that are extremely painful due to the belief that there is no other way to penetrate the extracellular material barriers. In 2020 a comprehensive study concluded that a pH-stabilized HOCl solution was able to reduce the amount of biofilms grown in vitro.
There are a abundance of peir ved and papers of We have mixed feeling concerning clinical trails so we took the long path of collecting real in vitro evidence. The more we collected the hugher or sales grew